Safe, Ethical, and Quality Eye Care
The College of Optometrists of Ontario exists to ensure that you receive safe, ethical, and quality eye care from any optometrist in Ontario. Here are some frequently asked questions about:
Eye Exams
What happens at an eye exam?
At most exams, the optometrist will note your health history related to eyes and vision. They will examine your eyes for any diseases or abnormalities. They will look at the way your eyes adjust to focus from near to far. The optometrist will also measure how sharp your vision is and if your eyes properly focus light. These things tell the optometrist if you are nearsighted or farsighted and how your vision compares to 20/20 vision.
Are eye exams covered by the Ontario Health Insurance Plan (OHIP)?
Eye exams are not covered by OHIP for most adults between 20 and 64 years old.
For patients 19 years and younger, 65 years and older, and those with certain medical conditions, OHIP covers a standard eye exam. As of September 1, 2023 there have been changes to which eye exams are covered by OHIP. The details of those changes can be found in this press release. If you have more questions about OHIP rules, contact the Ontario Association of Optometrists, OHIP, or the Ministry of Health.
Whether you are covered by OHIP or not, your optometrist may recommend additional testing at an extra cost. Before they do the test, they must:
- Explain why the test is needed in your situation
- Outline any additional fees and explain what they are for
- Discuss the benefits and any risks associated with the test
- Obtain your consent to perform the test.
Can I still receive the OHIP-covered eye exam if I don’t want the additional tests?
Yes. Additional testing and screening is not a condition of receiving the standard, OHIP-insured eye exam.
Why does my optometrist use eye drops?
Drops are part of many eye exams. The most common drops are used to dilate your pupils. This helps the optometrist better see the inside of your eye. These drops leave your eyes a little blurry and sensitive to light for a few hours. You may not be able to drive right after this procedure.
Other drops are used to relax the focus of your eyes. This helps the optometrist take certain measurements. These drops are generally used in children and young adults. They can also make the eyes blurry and sensitive to light.
Some drops are used to numb the eye. They are used when the optometrist needs to touch your eye with an instrument.
Finally, some drops contain a dye that helps the optometrist see abnormalities on the surface of the eye.
I hate the air puff thing. Is it necessary?
The air-puff test is one of several tests that can be used to measure eye pressure. This is an important part of an eye exam. It helps the optometrist determine your risk of developing glaucoma. If you find this test unpleasant, talk to your optometrist about other ways to measure your eye pressure.
Prescription
What information is included in a prescription?
A prescription for both glasses and contact lenses must include:
- the prescriber’s name, practice address, telephone number and signature,
- your name,
- the date of the eye exam, and
- all information that a licensed dispenser needs to make your glasses or fit the contacts.
A prescription will also include the power of each lens based on your specific condition: nearsightedness (myopia), farsightedness (hyperopia), blurred vision (astigmatism), or age-related need for reading glasses (presbyopia) – and may include additional information, such as magnifying power.
Contact lens prescriptions may also include information about a specific brand, material, size, or curvature of the lens depending on what you find most comfortable or is best suited to your condition.
Are lens prescriptions the same for glasses and contacts?
Sometimes the strength of your contact lens prescription may be different from your glasses prescription because contact lenses fit closer to the eye.
Will my optometrist automatically give me a copy of my prescription, or do I need to ask for it?
Optometrists must provide patients with a copy of their glasses prescription once it is ready and the patient has paid all the fees. Contact lens prescriptions are available following a contact lens fitting, and once the patient has paid all of the fees.
If you have health conditions that affect your prescription, your optometrist may not be able to provide a prescription until your vision stabilizes.
Where can I fill my prescription?
Any licensed dispenser can fill your prescription. This includes optometrists and opticians.
Glasses & Contacts
Should I buy glasses or contacts over the internet?
Buying glasses and contacts over the internet can be efficient and cost-effective for some people. But before you buy online, talk to your optometrist about your individual needs. People with complex prescriptions or certain conditions may find it hard to get a good fit online. This can result in glasses or contacts that don’t work, or even vision problems. We strongly encourage you to work with a licensed dispenser – an optometrist or optician – to be sure you’re getting the best fit.
Do glasses prescriptions have an expiry date?
Yes! Your prescription can change over time thanks to aging and medical conditions like diabetes, blood pressure, and cataracts, among others. If your eyesight is likely to change, your optometrist may recommend that your prescription not be filled after a certain date.
What is a contact lens exam?
Contact lenses come in a wide variety of designs, materials and sizes. A contact lens exam, which measures the shape of your eye and how moist your eyes are, helps find the best lenses for your vision needs and comfort.
A contact lens exam usually happens after a routine eye exam, when the optometrist knows your overall eye health and prescription needs.
Contact lens exams may require additional tests and may include a fitting fee.
I just want contacts to change my eye colour. Is it okay to buy them over the counter?
Cosmetic lenses sold over the counter do not correct vision problems, but they can still cause them. These problems including irritation and infection, if the lenses are not properly used and cleaned. Talk to your optometrist before using cosmetic lenses – they will be able to guide you on best materials, fit, and cleaning routines.
Roles & Responsibilities of Eye Care Professionals and Their Patients
What is the difference between optometrist, ophthalmologist, and optician?
An optometrist is a primary care provider – the first person you see about your eyes. They diagnose, treat, and manage conditions related to your eyes and vision. An optometrist can prescribe glasses and contacts, as well as drugs and treatments for certain eye conditions.
An ophthalmologist is a doctor who with specialized training in eye surgery, as well as diagnosing and treating eye diseases. Patients are usually referred to an ophthalmologist by their optometrist.
An optician is a professional who fits and adjusts eyeglasses, contact lenses, or other vision devices based on a prescription from an optometrist or ophthalmologist.
How do I know if I received good care from my optometrist?
You should expect that the care you receive meets the professional standards set by the College of Optometrists. Your optometrist must have the skills, knowledge, and judgment to practice in Ontario. You should expect to receive the information you need to make decisions about your health care. Your optometrist must respect the confidentiality of your health information.
If you receive glasses or contact lenses, you should be informed of the cost before the service is provided.
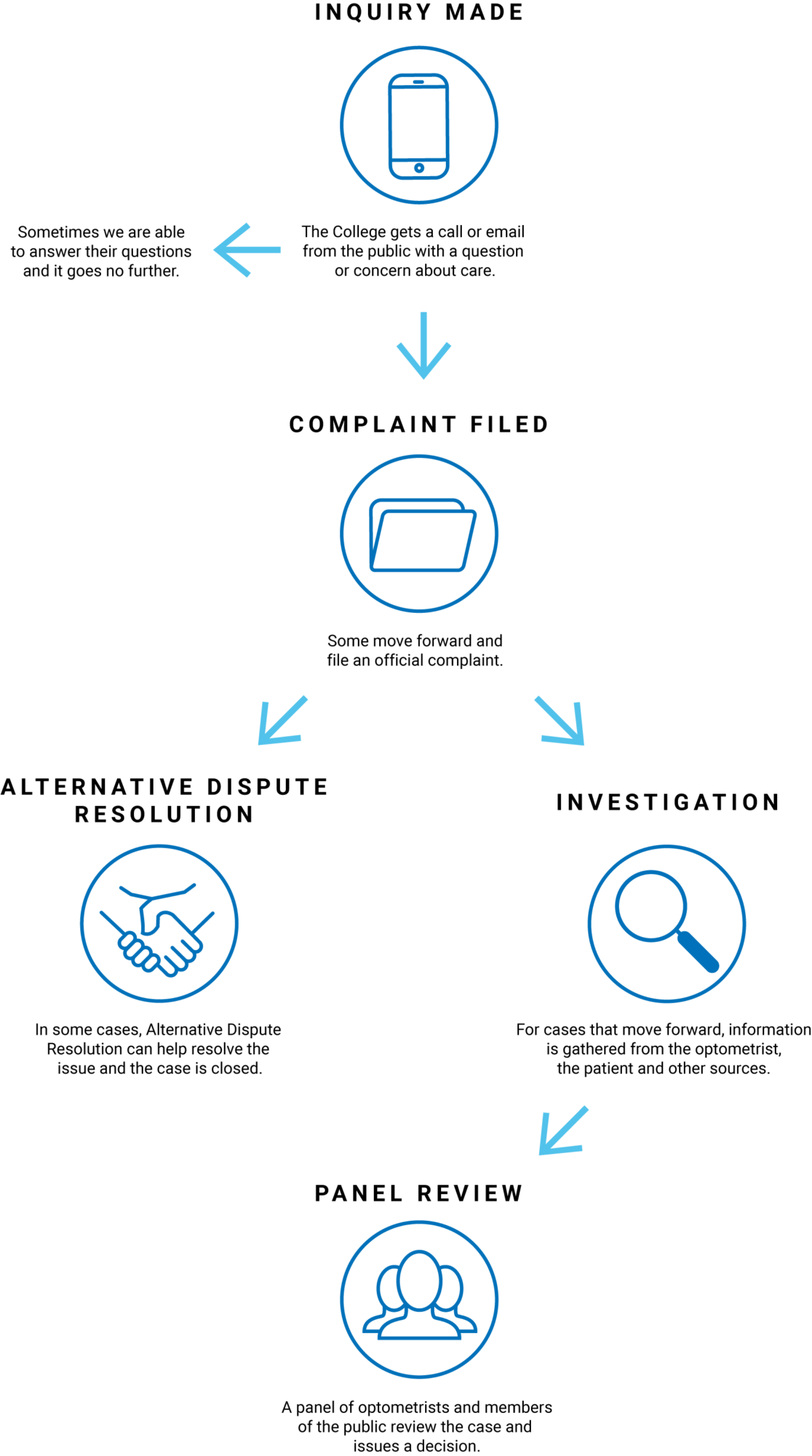
What if I feel I did not receive good care?
The first thing you should do is speak with your optometrist directly. If you are not comfortable doing this, or you did not get a satisfactory solution, contact the College. We can answer your questions and talk you through the formal complaints process. Learn more about reporting concerns and filing complaints.
What is the Assistive Devices Program?
The Ministry of Health and Long-Term Care pays up to 75% of the cost of low-vision aids through the Assistive Devices Program (ADP). Low-vision aids include:
- hand-held and glasses-mounted magnifying aids
- high-power glasses or lenses
- light filtering lenses
- technology such as large-print computers and text-to-voice applications.
A ‘registered authorizer’ is a person who can decide if you are eligible for coverage under this program. Some optometrists are both registered authorizers and approved vendors. That means you can receive your ADP funding and vision services in one place.
Visit our Funding Options for Eye Examinations in Ontario webpage to learn more about funding options for eye exams and vision aid..